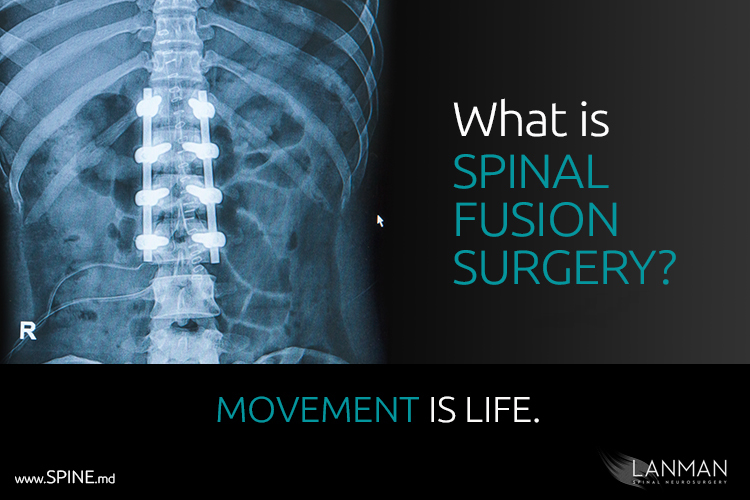
Spinal fusion surgery is a procedure where at least two vertebrae segments are permanently joined together with a highly-developed system of titanium screws, rods, and plates. A bone or synthetic graft is used to stabilize the vertebrae as one bone.
The main purpose of spinal fusion surgery is to prevent motion where a spinal disc has degenerated or ruptured. Bone graft material is added around the two segments. The graft may come from the patient’s hip or a bone donor. Some surgeons may use synthetic bone graft material. If all goes well, the graft will grow into the two vertebral segments and create the “fusion.” Once the patient is fully recovered, back and neck pain is gone thanks mainly to the fact that the vertebrae in the treatment area have been immobilized.
Spinal fusion was developed early in the 20th Century to help patients with tuberculosis, a severe life-threatening infection that often resulted in a condition known as scoliosis (curvature of the spine). In the 1940s, surgeons reintroduced the procedure to solve persistent back and neck pain. While the method has been nearly uniformly applied for degenerative disc disease for generations, it comes at a very steep price for the patient.
Since the goal is to prevent motion of vertebrae, the result is permanent limitation in the natural range of motion. This procedure may also trigger successive fusion surgeries due to the stresses that are added to other levels.
Other procedures such as laminectomy, discectomy, and artificial disc replacement have since been developed to give patients incremental options in the treatment of spinal disorders.
Laminectomies are often performed on an outpatient basis to treat patients who suffer from spinal stenosis, or a progressive narrowing of the nerve channels (the foramen). The surgeon can “clean out” the foramen so that the spinal cord and the nerve roots have more room (nerve decompression). Discectomies are also frequently offered on an outpatient basis. This procedure removes a small portion of a herniated spinal disc that is protruding and causing nerve compression, thus pain and numbness in the arms or legs. Discectomies (or micro-endoscopic discectomies) may be performed on any portion of the spine (cervical, thoracic, lumbar). In both cases – laminectomies and discectomies – may take 1 to 2.5 hours depending on the amount number of vertebral levels that require treatment.
Artificial disc replacement surgery (or total disc replacement) replaces spinal discs that have been herniated or ruptured. Currently, the procedure is approved by the FDA for the cervical (neck) and lumbar (lower back) regions of the spine.
Artificial disc replacement surgery (ADR, total disc replacement) was first developed in Europe in the 1980s. The procedure was later introduced into the United States in 2000 and has since undergone intense clinical study and subsequent FDA approval. After post-operative recovery, patients often report full restoration of their range of motion and flexibility. Post-operative recovery may often take as little as a week in some patients, up to 6 weeks.