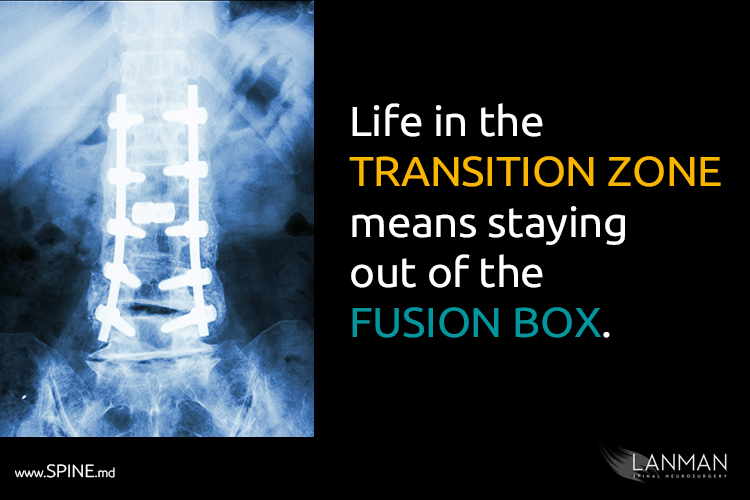
Why let pain drive you to desperate solutions that ultimately places you into the “fusion box”?
Konrad Bright lives an active life on the North Shore of Oahu, Hawaii. He’s been surfing all his life and is training in the martial arts. But one day, something went wrong. While enjoying one of those idyllic surfing days on the beach, excruciating pain shot through his lower back.
He initially believed he was experiencing a temporary pain that goes away after a while. The pain persisted for weeks, then months. There was also sharp shooting pain in his legs and a growing sensation of tingling and numbness in his toes and feet.
After suffering long enough, he met me at my practice in Beverly Hills, CA, and we discussed his situation. We performed an MRI scan and found the S1 disc, the base of the lumbar (lower back), was partially herniated.
Taking into consideration his active lifestyle, I suggested artificial disc replacement, which he rejected. To him, ADR was invasive surgery and therefore just as bad as spinal fusion. We discussed options—anything to keep from invasive surgery that Konrad feared would mean the end of his active life.
I agreed that microdiscectomy—a minimally invasive outpatient procedure—would give him immediate but temporary relief. I again suggested artificial disc replacement as a long-term solution. But Konrad had done his homework, which is not surprising. A recent Pew Research project found that 80 percent of American patients (about 93 million people) research their health options. Konrad was firm.
The microdiscectomy was a success. Konrad walked out of my office in Beverly Hills, pain free and just as flexible as he was before the herniated disc. However, the pain returned in six months and it was just as bad as it had been when we first met. A subsequent MRI showed what I feared would happen: the S1 disc had totally collapsed and the next level, L5, was also degenerating.
This time, Konrad knew his situation called for stronger measures. It didn’t take much to agree on a surgical plan that included a two-level artificial disc replacement. Despite his fears, soon after recovery he was back to all his former activities with full movement of his lower back. In fact, he was surprised how quickly he recovered—he was up in two days, and back to his activities in two months. Part of that fast recovery was due to his fitness. Had he undergone fusion however, his postoperative recovery would have likely stretched out to six months.
Konrad’s story has a great ending. Years later, and he’s still surfing those monster waves off the North Shore. How we met showed the seriousness he conducted his research and spinal fusion—the usual ‘go-to’ procedure for many surgeons—was definitely not for him. He was innately aware of what I call the “transition zone”—the place that spine surgery patients go before they engage additional surgeries. Like a growing number of patients, he also knew enough to avoid the “fusion box”—the place that often leads to more frequent surgeries and greater potential for post-operative complications like failed back surgery syndrome (FBSS).
I advocate for surgical procedures like artificial disc replacement because as a practicing neurosurgeon with more than 25 years of experience. My specialty is treating disorders of the spine. I’m also a professor at the University of California, Los Angeles, and a member of the Cedars-Sinai Institute of Spinal Disorders. And I either led or co-wrote the most often cited clinical research you will find on the internet showing spinal fusion often causing more long-term problems.
This makes sense structurally since we’re fusing vertebrae together—thus the name. Fusion puts a lot of pressure on nearby non-fused discs. The added pressure increases the likelihood for additional degeneration of adjacent discs and more fusion for other parts of your spine.
In one of my studies, my colleagues and I analyzed 19 clinical trials that involved over 4,500 patients. We concluded disc replacement surgery resulted in better functional outcomes, fewer adverse effects, and fewer surgical revisions than spinal fusion. Disc replacement patients also recovered quicker than fusion patients and saw fewer postoperative complications. And of course, disc replacement patient has a substantially better range of motion and better long-term outcome than fusion patients.
I must admit for some, few patients, multi-level spinal fusion may be the only viable answer. However, there are so many criteria a patient must reach before I will ever recommend such a course of action. Even as a patient reaches a point where fusion is inevitable, I always look for any way possible to keep them in the “transition zone.”
Life in the transition zone means we do all we can to maintain the natural flexibility of the spine for full and unrestricted motion potential for the body. We stay out of “the fusion box” for as long as possible and use minimally invasive procedures like micro-laminectomies and micro-discectomies to knock down marginal cases. These procedures are performed on an outpatient basis. You literally go home with less pain and, depending upon the extent of the surgery, you may even be able to return to your normal routine within days.
But surgery is not always the answer. In the transition zone, you may a fitness program that includes physical therapy and a nutrition program to strengthen your body from the inside out. We may focus on building your body’s ability to heal and make you more resilient to additional injury with body chemistry analysis, supplements, and asymptomatic disease screening.
Walk the transition zone with me, and I’ll spend a great deal of time discussing your family history, your daily routines at work, family life, hobbies, and anything else to flesh out the complete picture of how you came to end up with enough back or neck pain to want to see me. We’ll achieve two important goals:
First, I must learn how you became injured and treatments you have received. A thorough consultation helps bring me to a better understanding of how a disc was herniated and what, if any, surgery that was performed before you came to me.
Second, I want to know how long you’ve lived with this problem. I find that by the time patients are motivated enough to talk to a doctor about their condition, they have endured quite a lot of pain already. My consultation with you will let me know how you have tried to cope with the pain with over-the-counter medications or other measures.
But the most important aspect of living in the transition zone is learning about you, your body, and what it will take to make you greater than better.