Physicians run the risk of harming their patients with a 100-year old procedure.
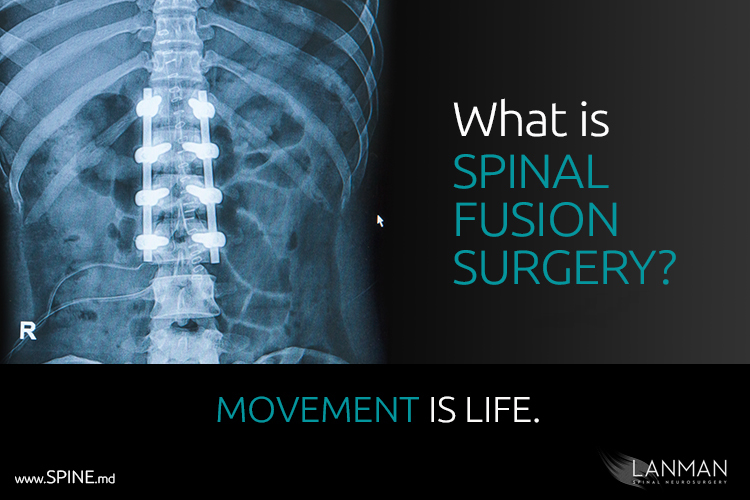
Compared with Artificial Disc Replacement, spinal fusion is an ancient and harsh solution for spinal disorders like degenerative disc disease and herniated discs. Not to be overly dramatic, but when I think of spinal fusion, I see the spine in a cage, restricted, confined, and trapped.
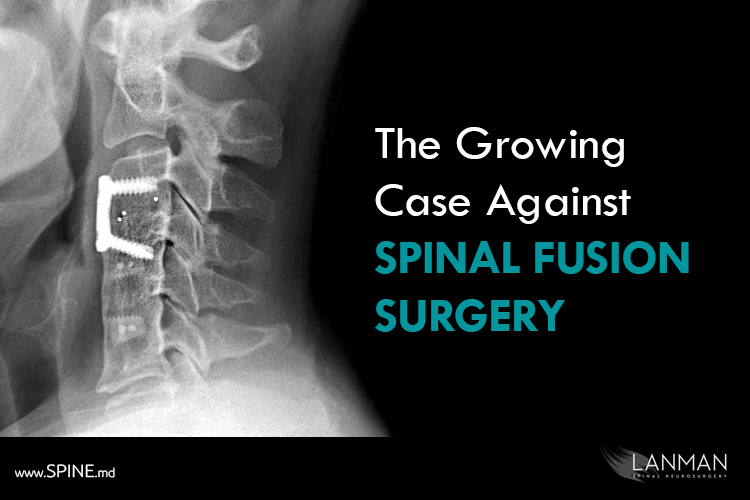
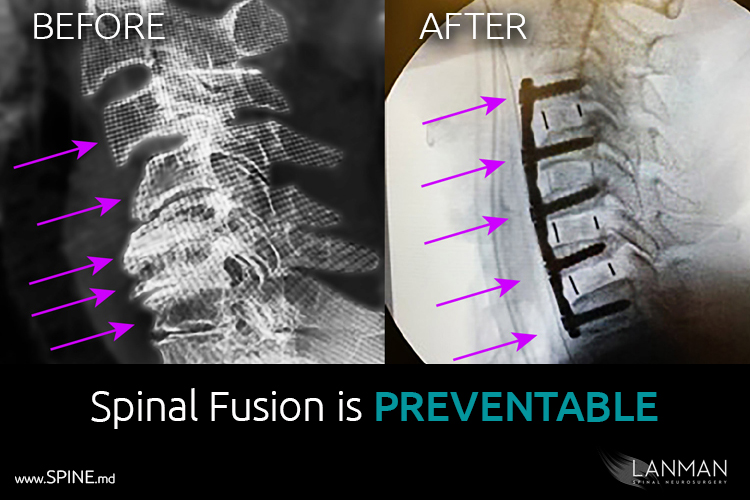
Spinal fusion is a mechanical solution to prevent the spine from moving. The purpose is to clear out fragments from a degenerating disc and stop bone from bumping into spinal nerves. This design philosophy is the complete opposite of artificial disc replacement where full range of movement is retained, while solving the pain issue. And we’ve been doing this successfully in the U.S. for twenty years, and more than thirty years in Asia and Europe.
So, why do so many U.S. physicians still recommend fusion for patients with appropriate spinal disorders? In my opinion, the reason is risk avoidance.
Many members of the medical community (not all) are what some business managers call “risk avoidant.” By avoiding risk, we reduce our exposure to potential problems and unforeseen consequences. There’s a good reason for rigidity in the practice of physicians. Imagine what would happen if any doctor could perform any procedure on any patient? What if we let doctors administer experimental drugs and try out untested methods? That’s the point of having agencies like the FDA. We may not like how it holds up medical innovations, but when they’re released and made fully available by the agency, you can be certain it has medical efficacy.
Moreover, it is our Hippocratic duty to “do no harm” to patients in our care. When we complete our training and accept our license to practice medicine, we pledge that we shall do our utmost to ensure that the care we offer is professional and ethical. And that’s how we arrive at the problem of spinal fusion.
Historically, when we had problems with the spine that couldn’t be solved with other measures, we turned to spinal fusion surgery. Back in the mid-20th Century, when a doctor prescribed fusion surgery, degenerative disc disease or other spinal problems had gotten so bad that severe nerve loss and functionality was a genuine threat.
For the most part, spinal fusion fulfilled a goal as an appropriate response for spinal deformities and instabilities back in the 1950s. Let’s pull in some perspective. Around the same time spinal fusion was reintroduced as a solution for herniated disc, medical scientists arrived at a method for the successful synthesis of penicillin, developed a vaccine for polio, and achieved the first successful human kidney transplants from a living organ donor.
Not to sound cliché, but that was then, this is now.
Not only has the FDA fully and completely approved artificial disc replacement for both cervical and lumbar applications, we’re already on to innovative artificial disc designs and new materials. More and more patients are receiving discs, and a greater number of them are enjoying long-term, problem-free outcomes.
It is puzzling to me that spinal fusion is still on the top of many physician’s treatment lists. According to several patients I’ve seen recently, a few physicians yet hold the old-fashioned opinion that artificial disc replacement is either experimental or not ready for everyone.
Are they being cautious, or is it something else? And what if the proclivity for caution is so erroneous that it invites harm? What if doctors pause at the open door of medical innovation, only to realize that they’ve lost the opportunity to do their very best to offer the best treatment available?
Let me be very clear. There is a problem, but it rests with our attitudes about what is accepted as “settled medicine.” Spinal fusion is a 100-year-old medical innovation. And there is a growing, substantial body of evidence showing that the new innovation is artificial disc replacement, for BOTH cervical (neck) and lumbar (lower back) applications. In repeated clinical studies that I and many of my colleagues have completed, ADR is proving itself with superior outcomes for disc herniation and spinal stenosis, especially where instability is not indicated. Based on my research and clinical studies by many of my colleagues, fusion is no longer an effective treatment of axial pain secondary to degenerative disc disease. And there is increasing evidence that fusion introduces severe foraminal stenosis and higher risk for adjacent disc herniations.
Bottomline message: it’s time to move on and embrace the new. Time to be Greater than Better.